HA Outstanding Staff
Year
Year 2021
1. Ms Leung Chui-ying, Ward Manager (Obstetrics & Gynaecology), PYNEH
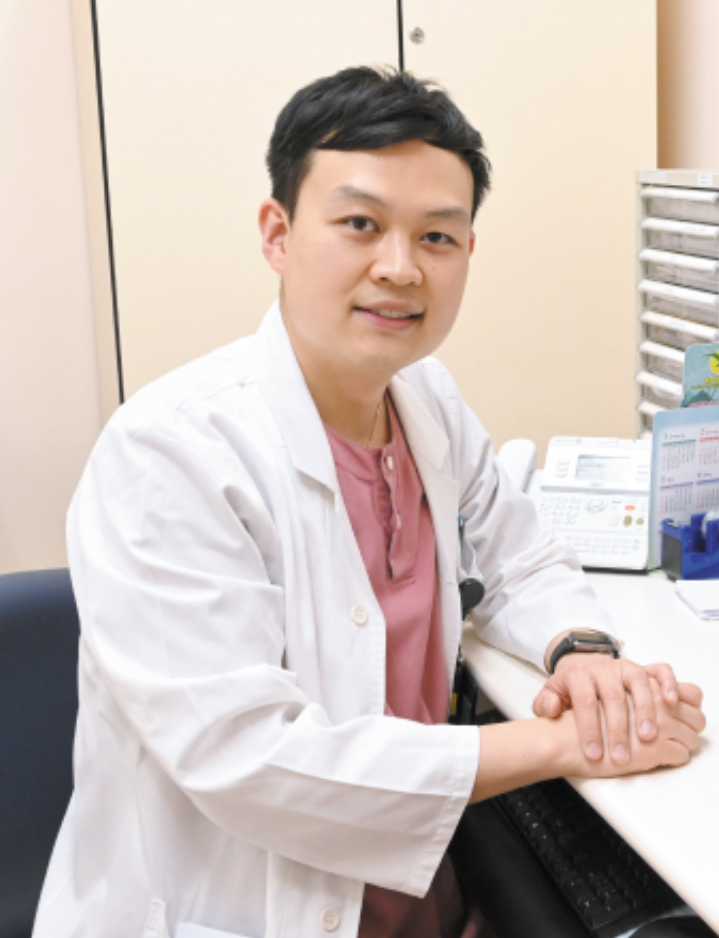
2. Dr Ko Tak-chuen, Consultant (Ophthalmology), PYNEH / TWEH
1. Ms Leung Chui-ying, Ward Manager (Obstetrics & Gynaecology), PYNEH
2. Dr Ko Tak-chuen, Consultant (Ophthalmology), PYNEH / TWEH
1.

Jade cannot glisten without being pondered and one cannot grow without pain.
After graduating as a nurse and the completion of a midwifery programme in the 90s, Leung Chui-ying joined in 1993 as one of the trail blazers for the Department of Obstetrics & Gynaecology of Pamela Youde Nethersole Eastern Hospital. In 1996, she participated in the establishment of semi-private wards, which were later used for hospitalising SARS patients when Hong Kong was hard hit by SARS in 2003. Chui-ying therefore led her team to combat the deadly virus. After the SARS outbreak, the semi-private wards were not re-opened so Chui-ying was assigned to support the medical emergency ward.
Her deployment as a nursing officer in medical ward gave rise to many doubts over her capability. “The first three months during my three years at the medical ward were the most challenging to me. However, I have acquired a valuable asset – the gist of people management.” Although days were tough, she remained steadfast and committed to overcome the challenges. “I used to skip lunch for a whole year just to familiarise myself with the patients’ clinical details. I had also once spent my nights to read over the user manual of a new model ventilator. When the doctor questioned how to use it, I was the only person who could operate it properly”. With an eagerness to learn, Chui-ying had proven herself a capable leader and eventually earned the respect from her colleagues.
In 2007, Chui-ying returned to the Department of Obstetrics & Gynaecology to commence the provision of private wards. Till 2020, she combated COVID-19 at the frontline with her team. Looking back, her days at the medical ward was a turning point of her life, where she emerged stronger from the new environment, and became a reliable leader among her colleagues and the pride of her family.
2.
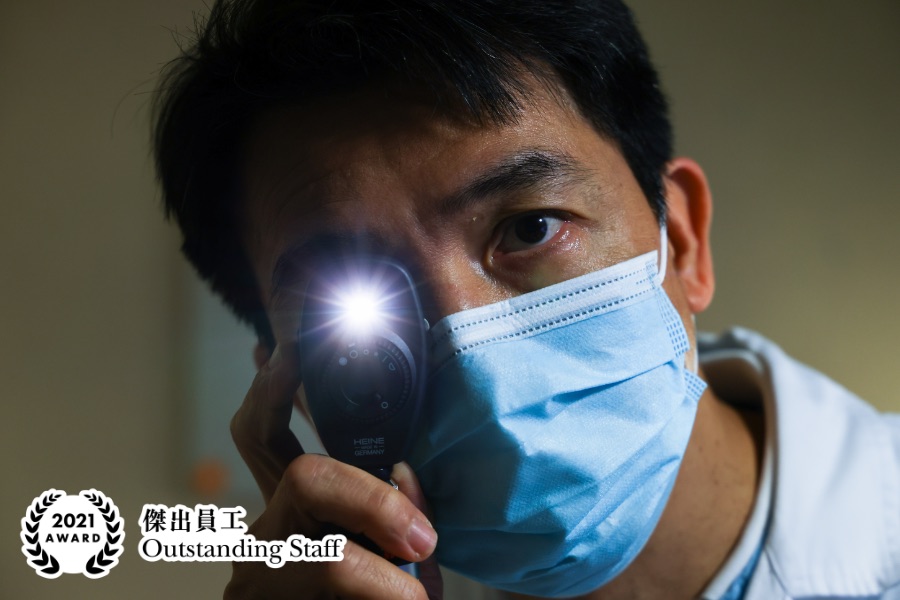
As the year advances, what we expect in medical services and how we train our people have been almost different from the way we did 30 years ago. Dr Ko Tak-chuen, who joined the Ophthalmology in Hong Kong East since 1990, believes that public hospital services must be tailored to the specific and prevailing circumstances. Dating back to the time when he devoted to the medical field, hospital beds were constantly in grave needs, whereas ambulatory care is broadly welcomed nowadays. The conventional approach to continuously providing more beds and strengthening manpower should no longer be the only solution. Additionally, making the best use of the currently available resources, or in other words, ‘re-engineering’ resources, is equally important.
Progress should not be made in only how we provide service, but also the way we think. “During my internship, I used to follow mentors and learn from the way they perform an operation. Nowadays, junior doctors would research for complex cases online and ask questions, thus I have to keep learning to achieve mutual learning goal with them.”
Dr Ko also puts emphasis on teamwork by valuing the opinions of his colleagues and thinking outside the box. Taking the Ophthalmology Service Enhancement Programme in the Hong Kong East Cluster as an example, “I was proposing that the Pamela Youde Nethersole Eastern Hospital and Tung Wah Eastern Hospital (TWEH) shall arrange day surgery for the patients with cataract and follow up hospitalised cases separately. However, my frontline team instead advised TWEH to be fully in charge of scheduling the surgery for patients from both hospitals. With the support from our administration and IT team, this suggestion can help prevent repetitive or missing follow-up cases as well as the redundancy in the manpower deployment, and to streamline the operation. In my opinion, their suggestion is more feasible, having considered that I may lack the hand-on experience of being at the frontline and getting in touch with the patients. Bearing this in mind, I always value the voice of my colleagues. With everything all set, the programme is expected to be implemented in the third quarter this year.”
Year 2020
Ms LEUNG Wai Ling, Department Operations Manager, PYNEH
Ms LEUNG Wai Ling, Department Operations Manager, PYNEH

Leung Wai-ling, one of the awardees of Outstanding Staff this year, has more than 36 years’ working experience in the field of obstetrics and gynaecology (O&G). She started her career as a midwife at Alice Ho Miu Ling Nethersole Hospital in Bonham Road and became a nurse educator of Nethersole School of Nursing for midwifery training since 1991. She later returned to the frontline at the O&G department of Pamela Youde Nethersole Eastern Hospital and in 2007, joined the nursing training school to teach registered nurses. She is currently the Department Operations Manager, a position she has held since 2011.
Reminiscing about her career journey, she feels blessed to have participated in patient care, education of the next generation of midwives, and drawing up the blueprint of the O&G department. But after all, the days in her life as a teacher are the most memorable of all. As Leung recalls, she shared the trivial things of life in the nursing school’s assembly, saying that she went to an amusement arcade to ease the pressure before going home to prepare the dinner. Thereafter, her colleagues (some of them were her students) still remembered this story and asked her if she still went to amusement arcade. She was therefore inspired that sprinkling her stories could help connect with students, which could be a good teaching approach. However, she says that she would be more delighted if her students remembered what she taught in the lessons and passed the knowledge to the next generation.
She says, “In the midwifery profession, I strongly believe that sharing experience with the younger generation is essential. Having said so, the attitude and mentality are crucial in nursing. I always remind my students and colleagues that, welcoming a newborn is an unforgettable experience for a family. To many mothers, the day they gave birth to their children is still fresh in mind even years later. For this reason, the company of a midwife plays a key role in the parents’ journey from pregnancy to delivery and enabling them to have a beautiful experience.”
Year 2019
Dr Eva Dunn Lai-wah, Consultant (Psychiatry), PYNEH
Dr Eva Dunn Lai-wah, Consultant (Psychiatry), PYNEH

A good psychiatrist is like a detective, says Dr Eva Dunn. To help a patient with mental health needs, a psychiatrist has to dig deep into a patient’s background, explore the symptoms, and talk to them at length to understand their inner world.
Dr Dunn launched psychiatry outreach services in the late 1990s, inspired by her belief that psychiatric treatment depends not only on medicine, but also support from the community where the patient lives. She worked with community psychiatric nurses to identify hidden and potentially high-risk cases and has been instrumental in increasing support for patients in the community through cooperating with the Social Welfare Department’s Mental Health Integrated Community Centre for Mental Wellness. The initiatives led by Dr Dunn have seen the establishment of recovery-based schemes for in-patients to help them reintegrate into community.
Dr Dunn initially wished to pursue a career in medicine, but incidentally joined psychiatry and was attracted. Having been a psychiatrist for 35 years, she has held major positions including Chief of Service (Psychiatry) at Pamela Youde Nethersole Eastern Hospital (PYNEH), Service Director (Mental Health) of Hong Kong East Cluster and Chairperson of the HA’s Coordinating Committees (Psychiatry). She champions culture change such as optimising psychiatric service delivery, strengthening risk management, promoting medical-social collaboration, and working with community partners on the concept of recovery. She has led her team to a number of awards including PYNEH Outstanding Team in 2005, and HA’s Outstanding Staff and Teams Awards (Merit) in 2006 and 2010.
As she prepares for retirement, Dr Dunn says she has a simple wish – for Hong Kong to become a mental health-friendly society where people work together to eliminate discrimination and allow patients with mental health needs to lead fulfilling and rewarding lives.
Year 2018
Dr YAN Wing-wa, Chief of Service (Intensive Care Unit), PYNEH
Dr YAN Wing-wa, Chief of Service (Intensive Care Unit), PYNEH
One of the outstanding staff of the year – Dr Yan Wing-wa is a leader with magnetic personality. Dr Yan started his career at Princess Margaret Hospital in 1986 and worked there until 2004 when he joined Pamela Youde Nethersole Eastern Hospital (PYNEH) as the Chief of Service of Intensive Care Unit (ICU). Over the years, Dr Yan has been awarded on multiple occasions as an individual and as part of a team. For instance, his team received the HA Merit Team Award in 2016 for their ICU Family Satisfaction Enhancement Programme.
It is the mission of a leader to keep the team together – a task that is easier said than done. But Dr Yan made it possible as the Chief of Service. The affable leader strives to establish a harmonious working environment and his approachable character makes his colleague ready to open up to him. “I believe a friendly relationship with colleagues helps build a strong team. Only when the team is united will my co-workers be ready to share their thoughts with me and accept my opinions.”
The interview was conducted in a handover meeting between the morning and afternoon shifts held by Dr Yan, during which everyone actively reported the updates of patients. Dr Yan explains, “The condition of patients in the ICU can fluctuate in seconds. Therefore, communication and understanding are critical to ensuring the best treatment for patients. Handover meetings are thus held every morning and afternoon. To enhance service quality, a sharing session has been added to the morning meeting in recent years, when young doctors are asked to share a medical article and answer questions from the floor.”
The prevalence of swine flu in 2009 is one of the most unforgettable incidents Dr Yan recollects. Dr Yan and his team tried to borrow an extracorporeal membrane oxygenation device to treat patients with lung failure. As a result, over 10 patients had their lives saved between October 2009 and August 2010 and the practice was subsequently adopted in other hospitals.
Moreover, Dr Yan and his colleagues have been urging that a hyperbaric oxygen therapy (HBOT) chamber to be installed to treat patients with decompression sickness, carbon monoxide poisoning, diabetic wound, necrotising fasciitis and avascular necrosis due to radiotherapy and improve their conditions. Dr Yan’s wish is fulfilled this year as the first HBOT chamber is installed in PYNEH. The facility will be brought into service later this year after testing.
Year 2016
Mr LEUNG Hung-foon, Chief Hospital Foreman, PYNEH
Mr LEUNG Hung-foon, Chief Hospital Foreman, PYNEH

Behind every hospital, there is a skilled ‘fixed-in-chief’ who can turn their hand to a multitude of rapid repairs and systems adjustments. Foremost among these multi-talented fixers at Pamela Youde Nethersole Hospital (PYNEH) is Chief Hospital Foreman Leung Hung-foon (Ah Foon).
Ah Foon worked in the Hospital Services Department in 1985 and joined HA in 1991 with the belief that the Hospital Authority was a vital new force for enhancing healthcare in Hong Kong. Later, he joined PYNEH on its opening in 1993, with responsibility for managing around 100 colleagues from cleaning and internal logistics to security and maintenance departments.
A naturally innovative and proactive person, he is particularly proud of two of his early initiatives that are still in place at PYNEH today. Suggested by the General Manager in 1994, the first is a ward-based preventive maintenance system that involves a routine monthly inspection of ward items and installations such as doors, desks, plumbing and ventilation equipment, in order to deal with potential problems before they become major issues. Ah Foon is also the brain behind the establishment of a Central Control Room at the hospital, which serves as a one-stop shop for all supporting services, including cleaning, internal logistics, monitoring of the security system and the alarm system, the key management system and quarters management.
Due to retire at the end of this year, Ah Foon says, “If you work in wholehearted and sincere way, being a foreman is a meaningful job. My most unforgettable experience was on 28 February 2000 when a bomb was found on the third floor of East Block in the psychiatric ward. Following the instructions of the Police to evacuate, we had to move around 400 psychiatric patients from confinement wards to the rooftop as quickly as possible. This was a huge challenge, as, in addition to being unable to take the elevator and making sure that the patients were accounted for at all times, we had to try to keep everyone’s emotions stable. Fortunately, we were successful in our endeavours and the incident was resolved without anyone getting injured.”
Ah Foon was lucky enough to also find romantic happiness at PYNEH. In his early days at PYNEH, Ah Foon met his wife, who was a matron of the hospital’s staff quarters. The couple has now been married for many years.
Year 2015
Mr Andy Lam Hing-kuen, Mortuary Officer, PYNEH
Mr Andy Lam Hing-kuen, Mortuary Officer, PYNEH

It was while working as a Clerk II in the Department of Pathology at Kwong Wah Hospital that Andy Lam, a liberal arts secondary school graduate, gained the knowledge of biology and human anatomy that enabled him to move into his current career in mortuary services.
In 2009, Andy joined the Clinical Pathology Department at Pamela Youde Nethersole Eastern Hospital (PYNEH) as a Mortuary Officer. Currently, he also helps coordinate the mortuary services in the Hong Kong East Cluster, besides working for PYNEH.
Andy credits his religious faith for his ability to work in an environment that might spook many others. “My beliefs dispel any fear of ‘ghosts’ or ‘spirits’,” he says. “Very often I’m the last staff to leave the mortuary in the evening. I’m passionate about my job as I truly believe I’m helping people.”
In a bid to create a supportive environment for bereaved family members, he helped the department in setting up the Peaceful Hall where bereaved families can bid farewell to their loved ones; and the Bereavement Room which helps families in body viewing and identification.
In 2010, Andy helped Hospital Authority successfully implement the Radio Frequency Identification (RFID) system. RFID is an effective tool in ensuring that bodies under mortuary care can be easily identified, tracked and managed. The system has now been adopted by 12 hospitals of HA.
In retrospect, Andy is delighted that the perspective of a career in mortuary services by the public has changed. “People used to think that those who work in mortuaries are old or of low education. In fact, all of my colleagues are educated to Secondary five or above and the average age here is around 30. Our youngest colleague, a mortuary assistant, is only 23!”
Year 2007
Dr Lau Chor-chiu, Cluster Service Director (Clinical Services) / Clinical Coordinator (A&E), HKEC & Chief of Service (A&E), PYNEH
Dr Lau Chor-chiu, Cluster Service Director (Clinical Services) / Clinical Coordinator (A&E), HKEC & Chief of Service (A&E), PYNEH
Totally committed to providing holistic care to patients through high quality Accident and Emergency services, Dr Lau Chor-chiu has made tremendous contribution to his specialty, the medical profession at large as well as the community.
Dr Lau believes patient-centred communication is the key in the pursuit of quality care and professional development. He has partnered with Human Resources in pioneering tailored made training programs for A&E doctors and nurses. He also rendered significant contribution in the development of Hospital Trauma Policy and multidisciplinary protocols to ensure efficient trauma management and reduce unnecessary A&E re-attendance and ward admissions. As the current president of the Hong Kong College of Emergency Medicine (the College), Dr Lau provides visionary leadership in developing new skills and new interests in clinical management modalities to keep pace with emergency medical services.
Serving as Senior Air Medical Officer in the Government Flying Service (GFS), Dr Lau plays a crucial role in extending emergency medicine outside the hospital. In 2004, Dr LAU courageously took up the mission to render assistance to the victims of the Jiufen traffic accident and the Hong Kong tourists affected by the tsunami in South Asia. His brave act has demonstrated the professionalism of clinicians and also reinforced the positive image of the HA.
Year 2005
Dr LI Ka Wah, Michael, Chief of Service (Surgery), PYNEH
Dr LI Ka Wah, Michael, Chief of Service (Surgery), PYNEH

Dr Li is the pioneer of minimal invasive surgery (MAS) in Hong Kong and is highly regarded as a prominent figure in the surgical field. He has established the Minimal Access Surgery Training Centre in PYNEH and succeeded in founding the first global Endo-laparoscopic Theatre in January this year. This brand new concept brings a great leap forward in MAS development.
With his excellent leadership, Dr Li has built up a very professional and efficient surgical team in PYNEH. He shows great concern for the career development of his subordinates and spends tremendous efforts in training them and actively involving them in research work. Dr Li’s outstanding achievements are well respected by his colleagues, patients, public and international parties.
Year 2004
1. Mr Cheng Kai-chi, Administrative Assistant, PYNEH
2. Dr Yam Yin-chun, Loretta, Chief of Service (Medicine), PYNEH
1. Mr Cheng Kai-chi, Administrative Assistant, PYNEH
2. Dr Yam Yin-chun, Loretta, Chief of Service (Medicine), PYNEH
1.

Despite of being an administrative assistant, Chi 's contribution is totally beyond his position. Chi is very competent and capable to take charge of two units, namely the Medical Media Unit and Minimal Access Surgery Training Centre, in an effective and efficient manner. His technical expertise contributes towards enhancing audio-visual facilities of the Hong Kong East Cluster. His positive working attitude and commitment to work is highly admired by colleagues.
2.

Dr Yam has made enormous contributions to the medical profession. She always demonstrates a strong commitment to her work and is dedicated in training and coaching staff members. She took the lead in different resources management programs which set good example for other clinical departments. With her superb leadership and professional knowledge, she led her cohesive team to fight the battle tirelessly during the SARS crisis.
Year 2001
Ms CHEUNG Sau-fong, General Manager (Nursing), PYNEH
Ms CHEUNG Sau-fong, General Manager (Nursing), PYNEH

Ms Cheung has contributed substantially to the establishment of the nursing culture, enhancement of staff's training and departmental communication. She is an advocate on patient care and makes optimal use of resources especially during hard time. Under Ms Cheung's leadership, her nursing team strives the best to improve service quality and is always willing to participate in pilot projects and new challenges. Recently, the nursing team has accredited the ISO 9002 certification.
Year 1996
Mrs Wan Yeung Kam-shim, Mary, General Manager (Administrative Services), PYNEH
Mrs Wan Yeung Kam-shim, Mary, General Manager (Administrative Services), PYNEH
Mrs Wan Yeung Kam-shim, Mary, General Manager (Administrative Services), PYNEH
Mrs Wan is a champion of cultural change who has scored outstanding achievements. She has succeeded in changing the culture and mentality of her subordinates, so that they all consider front-line staff as their customers and provide customer-focused administration services. In turn, other staff are empowered to provide quality care to patients. She initiated her Hospital's successful pursuit of ISO 9002 Certification for Materials Management and Human Resources Services.
Mrs Wan is a champion of cultural change who has scored outstanding achievements. She has succeeded in changing the culture and mentality of her subordinates, so that they all consider front-line staff as their customers and provide customer-focused administration services. In turn, other staff are empowered to provide quality care to patients. She initiated her Hospital's successful pursuit of ISO 9002 Certification for Materials Management and Human Resources Services.
HA Outstanding Teams
Year
Year 2025
HKEC Stoma and Wound Care Team
HKEC Stoma and Wound Care Team

Hong Kong East Cluster
“If I were the patient, what kind of help would I hope to get from healthcare professionals?” Putting themselves into patients’ shoes and meeting patients’ urgent needs, it is this belief that motivates the Hong Kong East Cluster Stoma and Wound Care Team to innovate continuously. The Team is dedicated to managing post-operative wounds and was founded in the 1990s by the Department of Surgery at Pamela Youde Nethersole Eastern Hospital. This led to the establishment of the Stoma and Wound Nurse Clinic, which constantly explores and pioneers new nursing technologies.
In 2009, the Team became the first in Hong Kong to adopt Woundoscopy – a technique that uses endoscopy to assess wounds – and utilise iPad to analyse the colour of wound fluids to allow for more precise care. The Team has also been a pioneer in Point-of-Care Ultrasound since 2018 for the examination of wounds, stomas, and gastrostomy tubes. Patients who undergo gastrostomy surgery rely on tubes for enteral feeding afterwards. Previously, around 20% of patients experienced tube dislodgement who required emergency hospitalisation. “We were the first in Hong Kong to use ultrasound to ensure the correct placement and alignment of the gastrostomy tube and to check the size of the balloon inside the stomach that secures the tube to prevent dislodgement,” the Team explains. After the implementation of the advanced nursing practice, the number of dislodgement cases in Surgical Department has dropped to zero and complications related to gastrostomy tubes have decreased significantly.
In one notable case, a female patient suffered from peristomal granuloma – unhealthy tissue growth around the peristomal skin – causing severe pain that kept her awake at night-time. The swollen granuloma was prone to bleeding, adding to her anxiety. Drawing on lessons from haemorrhoid ligation by surgeons, the Team developed an innovative technique to ligate the granuloma with surgical sutures, allowing it to gradually shrink and eventually disappear. “This technique is far from easy. We practised it repeatedly, and the procedure requires close collaboration among team members to be successfully carried out,” the Team explains.
“Achieving breakthroughs from zero to one requires far more time and effort than making incremental improvements from one to two.” The Team remains committed to continuing to advance wound care standards and is dedicated to passing on expertise and encouraging innovation by the emerging generation of young healthcare professionals.
Year 2024
Robotic Surgery Team - PYNEH
Robotic Surgery Team - PYNEH

Advances in medical technology mean procedures that could not be conducted by minimally invasive surgeries in the past can now be broken through and successfully carried out by robotic surgery. Pamela Youde Nethersole Eastern Hospital (PYNEH) established the world’s first Robotic EndoLap Operating Room in 2009, which also acts as a training centre and a platform for global experts to exchange skills, including cross-cluster operation and training support, live surgery demonstration, organisation of workshops and international conferences.
The robotic surgery team has far greater capabilities and more mature techniques in advanced surgery than when it was established 15 years ago. Initially, robotic techniques were applied in urological, gynaecological and general surgery. Technological advancement has allowed robotic surgery to overcome the limitations of minimally invasive surgeries and be used in complex procedures, such as radical prostatectomy, total mesorectal excision, hepatectomy and pancreatectomy.
“Robotic surgery system provides three-dimensional and high-resolution imaging. The robotic arm imitates the human wrist joint design and can even perform a 360-degree rotation, making great advantage in the dexterity. It is especially suitable for tissue dissection and anastomosis reconstruction.” More than 3,600 operations had been performed in PYNEH by the end of last year.
Surgeons are required to undergo training to understand how to use robotic equipment and then assist credentialed surgeons for some time before performing robotic surgery under supervision. Operating theatre nurses support the development of robotic surgery by providing training for counterparts in local public and private hospitals, the Greater Bay Area and also Southeast Asia. “The high level of cooperation among surgeons, anaesthesiologists, and nurses in robotic surgery is like a Formula 1 race. When the car drives into the pit stop, everyone performs their duties smoothly and accurately. Even if there is an equipment failure or a change in the patient’s condition, teamwork can solve everything.” The Team hopes to have more opportunities to exchange knowledge with global experts and handle a broader variety of cases as it continues to set new standards in the field and improves the training system.
Year 2023
Hong Kong East Cluster End-of-Life (EOL) Community Care Project Team
Hong Kong East Cluster End-of-Life (EOL) Community Care Project Team

Set up in 2016, the HKEC End-of-Life (EOL) Community Care Project Team brings holistic care to end-stage patients with cancer or chronic illnesses through medical-social collaboration (MSC), caring for their body, mind, social life and soul. “The final journey of life is not necessarily black in colour. Adding some colours may make it more joyful. In many cases, other than reducing pain through treatments, what they need most are spiritual care and support in daily life.”
Through MSC, healthcare staff take care of patients’ medical needs, while community partners take care of their psychosocial needs and daily life, or even fulfilling personal wishes. “It is quite hard for doctors and nurses to fully understand patients’ thoughts and needs in a short period of time. We thus collaborate with community partners to provide boundless care regardless of location,” the Team explains. “Once, a patient wanted to eat roast goose with her husband in Sham Tseng one last time. It sounded simple but was difficult due to her limited mobility. Her wish was finally fulfilled with the help of volunteers.” In order to help community partners understand diseases and facilitate them in providing daily care to patients, the Team also provides them with healthcare knowledge.
Under the project, both parties collaborate to tailor the most appropriate treatment and care plan for patients. Each patient is assigned with a link nurse who facilitates close communication between both teams and regularly reviews the latest condition. There was once an elderly woman, suffering from end-stage chronic obstructive pulmonary disease, worried that her husband, who also had difficulties in self-care, has to take care of her if her condition is deteriorated. The social worker then explored different EOL treatment options with the patient. “She proposed to sign the ‘Do Not Attempt Cardiopulmonary Resuscitation’ consent form. She said it was a thoughtful decision and felt relieved after signing. We were also glad to make the arrangements according to her wish.”
Facing ageing population, the Team hopes to further promote this service model which leverages resources of both the hospital and community to provide a more holistic care to patients. “With support from community partners, we can rest assured that patients will still be well taken care of after stepping out of the hospital and we can concentrate on medical treatments. There may not be much time left for the end-stage patients but we hope their voices can be heard, and they can enjoy their final journey.”
Year 2022
Hong Kong East Cluster Urology Team
Hong Kong East Cluster Urology Team
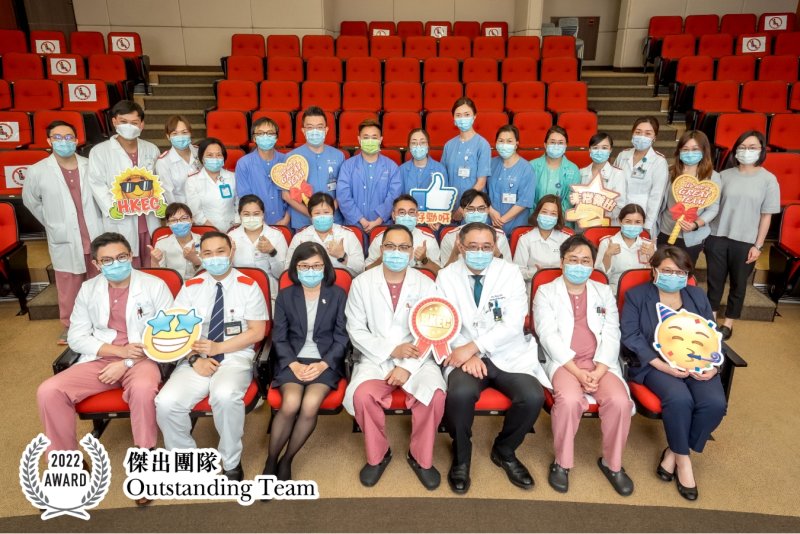
Dealing with delicate personal problems such as dysuria, erectile dysfunction, and urinary incontinence with the best solution requires patience and perseverance from members of the Hong Kong East Cluster Urology Team. “It is because you care about your patients that you are willing to make changes to improve their quality of life, but taking that step involves a degree of inquisitiveness,” explained by the Team. “You don’t know if you will succeed unless you give it a try.”
The Team often finds patients in a dilemma. In one case, a middle-aged patient suffered from dysuria wanted to give up the trial of his catheter removed due to the pains after removal. However, as the family’s breadwinner, he was reluctant to continue wearing a urinary bag. To address his concerns, the Team coordinated with the outpatient clinic and ward to allow the patient to stay in the clinic longer than usual for observation. Each time he felt unwell, the Team took follow-up action immediately, and his condition was cured within a fortnight.
“You can change a patient’s life if you are willing to go the extra mile,” members of the Team argue. “Urinary catheter insertion has been commonplace, but the inconvenience it causes is often overlooked.” The Team has established a set of Trial Wean-Off Catheter guidelines with streamlined caring procedures, allowing different departments to help suitable patients wean off catheter. “The departments are always busy, but Team members were willing to work on the guidelines and even spent their spare time discussing each case,” the Team members say.
Nurse clinics have also been set up by the Team to arrange preliminary investigations, enabling better triage and continuous follow-ups on patients’ needs, with nurses directing their efforts toward the patients they are best able to support. “For example, male patients are more comfortable talking to male nurses about erectile dysfunction, while female nurses can deal with female patients’ incontinence, making it easier for them to build mutual trust,” the Team explains.
Breakthrough is not just about deploying the most advanced surgery and services, according to the Team, but finding ways to address each individual patients’ needs and being more persevering even than the patients themselves.
Year 2021
1. COVID-19 Patient Management and Support Team - PYNEH
2. Minimal Access Surgery Training Centre - PYNEH
3. Implementation of Drug Refill Services (DRS) in HA - HAHO / NTEC / NTWC / HKEC / KEC
1. COVID-19 Patient Management and Support Team - PYNEH
2. Minimal Access Surgery Training Centre - PYNEH
3. Implementation of Drug Refill Services (DRS) in HA - HAHO / NTEC / NTWC / HKEC / KEC
1.

During the COVID-19 outbreak, Hong Kong East was once the ‘hardest hit area’. Over 1,000 colleagues from various departments of Pamela Youde Nethersole Eastern Hospital, including Obstetrics and Gynaecology, Surgery, Orthopaedics and Paediatrics, took turns to lend a helping hand to the Medical wards. Among both colleagues and patients, everyone has gone from strangers to comrades-in-arms, fighting the pandemic together.
The team leader Dr Lung Kwok-cheung, who is also a Consultant of Department of Medicine and his team members have this to say, "We come from different departments, but we are all united in our mission to put the well-being of our patients first. And it is a good opportunity for colleagues to share their experience. For example, the Medical wards received many confirmed patients aged from a few months to a few years. We were not overwhelmed only with the help of Paediatrics colleagues. Of course we reciprocated by showing how to care for older patients which we are good at.”
Colleagues become comrades, while the patients see love in times of adversity. “The team attaches great importance to the 'family' culture. We try to arrange COVID-19 patients from the same family to stay in the same cubicle so that they can take care of each other. For patients who are 'solo' (i.e. being admitted to the hospital alone), we will arrange beds flexibly. For instance, a few little girls were admitted to the hospital earlier this year. So we asked another older girl to stay with these younger ones and take care of them. When they were discharged from the hospital, they were a little sad to leave each other. Another old lady did not want to stay in a single cubicle as she was scared of ghosts and the dark. In the end, some young female patients volunteered to stay with her. After assessment, we agreed to this arrangement and the ladies even fed her soup and helped cut her nails. We were surprised that the patients went from being strangers to friends.”
Dr Lung was pleased to receive the award, but he wished the team could be disbanded because it means the end of the pandemic, and everyone’s lives return to normal. He is convinced that even if the pandemic subsides, the rapport that the team has built will go on.
2.

In early 90s, when minimally invasive surgery was newly introduced to the medical field, surgeons predominantly adopted conventional open surgery. Dr Michael Li, Founding Director of Minimal Access Surgery Training Centre, had the foresight that minimally invasive surgery (MIS) would be the dominant trend and subsequently established the centre in 1995 with the support from Hospital Authority and the management of the hospital.
Director of the Centre, Dr Tang Chung-ngai recalled when the Centre was first established, the minimal access surgery training was conducted in a small room with very basic equipment. Nevertheless, every training session attracted over dozens of participants, who showed keen interest in this revolutionary trend. Thanks to the support from Alice Ho Miu Ling Nethersole Charity Foundation, the Centre was expanded and installed with EndoLap Operating Room (EndoLap OR) and advanced computer simulation equipment. Its renovation followed in 2017 to facilitate the provision of various surgical trainings with state-of-art devices and video equipment, as well as robotic surgical training. With Simulation Operation Room (Sim OR) in place, cross-disciplinary simulation training is also provided to improve team communication and coordination.
The Centre has been engaging in various local and overseas exchange programmes to promote the development of MIS and nurture young surgeons. With such opportunities, Hong Kong is playing a more pivotal role under the international spotlight. The Centre has so far organised around 450 training courses for over 16,000 participants, among which 70% are local healthcare workers, while the remaining are from overseas medical institutions.
The contribution from predecessors in pioneering MIS has laid important cornerstones for subsequent development. Yet, the challenges arisen in the course of the Centre’s development, including sustainable quality teaching, team coordination, people management and resources allocation, could only be overcome with the team’s unwavering determination. What the team has accomplished by far most strongly testify to the team’s hard work and perseverance over the years.
3.

To reduce the risks of drug surplus and drug misuse among specialist outpatients, the HA Head Office and four clusters have jointly launched a pilot programme on ‘E-fill’ Drug Refill Services since 2017 to consolidate and refill drugs for eligible medical outpatients in phases. As at April last year, about 20,000 patients have benefited from the programme. The team describes the process as an endeavour in continuous improvement and the results today have not been easy to achieve.
Teresa Ngan, the team leader and Senior Pharmacist, and her team members explain that the programme seems simple to execute, as it only requires patients or their families to collect refill medications at designated counters of hospital’s pharmacy according to the refill schedules on the prescription slips. In fact, it involves cross-hospital, inter-departmental and multi-disciplinary participation. The process is constantly modified in the light of clinical experience, and technological elements are incorporated to pave the way for the future development of Smart Hospital pharmacy services. These include the setting up of computer systems and the use of big data to screen eligible patients, the establishment of messaging channel between the Clinical Management System and the Pharmacy Management System, as well as the digitalisation of drug collection.
The service has also strengthened the role of pharmacists in multi-disciplinary collaboration. Under the programme, pharmacists will review upcoming prescriptions daily and reconcile the relevant patients’ medications. They will call patients or arrange face-to-face consultations if the patients are found to have been admitted to hospital or need prescription changes. The members say, “As doctors have limited time for consultation, if pharmacists can communicate with patients in advance, they can share the workload of doctors in reviewing prescriptions during consultation, and at the same time patients can understand more about use of medication, which is a win-win situation. The programme has also led to many opportunities and planted the seeds for future development under the new normal of healthcare service. So our colleagues are getting more and more engaged in it.”
Year 2019
Hong Kong East Cluster Environmental Management Team
Hong Kong East Cluster Environmental Management Team

The ‘20-year eco-challenge’ memes spread across Hong Kong East Cluster (HKEC) deep and wide. HKEC Environmental Management Team makes ‘go green’ a lifestyle, a paradigm shift and culture in the cluster, and perfectly exemplifies various initiatives at hospital level. With the aim to stop the depletion of resources, pollution and exploitation of the world, the team demonstrates HA’s vision of ‘healthy people’ with profound effort.
Energy management and reduction of electricity consumption in 1997 was the first step of going green in HKEC. Eric Wong, Cluster Manager (Facilities Management), explains that huge amount of energy is required to support 24-hour medical services in hospitals, covering lighting, air conditioning, and operation of medical equipment. Currently, HKEC consumes over 100 million units (kWh) of energy each year, about half of which comes from air conditioning and ventilation system. “Today, in addition to replacing high-efficiency chiller units, a central energy management system is also required to monitor electricity usage throughout the day. Regular and frequent inspection of temperature at different zones of the hospital is also essential.”
The Central Production Unit responsible for handling patient food services in nine hospitals also rolled out a campaign in 1997 to reduce food waste. As some patients were in fasting and some preferred home-cooked meals prepared by family, the hospital decided to allow nurses to instantly update and input the required amount of patient meals through a notification and computing system. On the other hand, the laundry, handling 55,000 pieces of clothes and linen a day, redesigned the curtains with fabric 40% lighter and reduced the size of bath towel by 20% to lower water consumption in recent years.
Department renovation provides a good chance for environmental conservation drives. To achieve optimal use of energy during non-service hours, an energy saving mode or ‘night’ mode function was installed in the ventilation control system of the ophthalmology operating theatre in Tung Wah Eastern Hospital during renovation. Department of Clinical Pathology of Pamela Youde Nethersole Eastern Hospital also reviewed its setting and applied the latest ventilation standard in the laboratory. “The old air ventilation system continuously supplied 100% fresh air with zero return air to meet the then standard of infection control when the hospital was designed. With a high standard of air filtration level and circulation function, the new system requires only 30% supply of fresh air to maintain air quality, thus greatly reducing energy consumption,” Department Manager Albert Li elaborates.
Julie Li, the team leader and Cluster General Manager (Administrative Services) of HKEC explains three unique attributes of HKEC in its energy saving drive, namely sustainable culture, active participation of staff, and the integration of green drives in daily work, be it clinical and non-clinical. “We often encourage colleagues to express their ideas and suggestions on environmental protection. Ideas, if adopted, will have strong administrative support. In manifesting our social responsibility, the cluster successfully translates HA’s vision into environmental-friendly actions with a green culture that stands the test of time. We are proud of HKEC,” she adds.
Year 2017
Chai Wan Laundry, PYNEH
Chai Wan Laundry, PYNEH

“We provide thoughtful support to colleagues and patients by improving the design and material of clothing, and simplifying the workflow.”
Chai Wan Laundry is awarded Outstanding Team 20 years after winning the award for the first time in the year 1997/1998. Karen Lee, the team leader and laundry manager, shares about her thoughts and feelings, “We are overjoyed! Winning the first prize was a turning point to us ﹣ it represented that our team was ready for new technologies. And this second award recognises our successful integration into the era of automation. All of us are open to new knowledge and innovative thinking so as to modernise the laundry.”
Karen says, “The work in a modern laundry is more than washing and sterilisation. We think innovatively from the perspectives of users and our team members, to develop unique clothing designs and to simplify the workflow as a whole, aims to bring staff and patients convenience.” To stimulate innovation, Karen often encourages colleagues to enrich themselves through joining training courses on textiles, management or applying for a boiler license.
“Clothing is like the second skin. We hope our users feel comfortable in their clothes as they work or receive treatment.” Karen also reminds colleagues to check pockets before sending their clothes to the laundry. “We often find bits and bobs like ball pens, chops, pagers and tissues. Once a ball pen crushed a component of the washing machine, bringing the whole work process to a halt as we need to replace spare parts of the machine.”
Laundries under HA are mainly responsible for handling hospital clothing items, such as bed sheets, ward curtains, patient clothing and staff working clothes.With an area of 2,000 square metres, Chai Wan Laundry is responsible for hospital Clothings of the Hong Kong East cluster, Kwong Wah Hospital and Tseung Kwan O Hospital, handling around 55,000 items daily.
Year 2015
Hong Kong East Cluster Wound Management Team
Hong Kong East Cluster Wound Management Team

Drawing on the strengths of a multidisciplinary approach to health, Hong Kong East Cluster’s (HKEC) Wound Management Team has developed a three-tier wound management model that significantly cuts 14% of the wound redressing frequency, and the average healing time for chronic leg ulcers has dropped 44%.
In 2009/10, for example, the ratio between wound redressing attendances and patient headcount in the cluster’s General Outpatient Clinic (GOPC) was 4.5. By 2013/14, this had fallen to 3.86. The average healing time for chronic leg ulcers at the cluster’s GOPCs has dramatically fallen from 74 days in 2009 to just 41 days in 2012.
“Multidisciplinary collaboration has helped us achieved standardisation of wound and pressure ulcer services across the cluster’s hospitals,” explains Dr Sy Chung-tai, core member of the Working Group and Associate Consultant of Pamela Youde Nethersole Eastern Hospital. “This ensures that patients will benefit from continuity of care even if they are transferred to another HKEC hospital or require post-discharge follow-up consultations by our Community Nursing Services.”
The Working Group’s efforts have won endorsement from the European Wound Management Association and they are currently the only group in Greater China accredited to provide advanced level wound management training. They continue to innovate and pursue higher levels of excellence. Ho Chi-wai, Nurse Consultant (Wound & Stoma Care) and core member of the Working Group, has developed the woundoscopy – a wound assessment technology that has enhanced surgical accuracy by enabling better assessments of wound beds. He has also leveraged an existing iPad app to create a wound exudate assessment tool that gives clinicians more information to evaluate the need and urgency for invasive wound treatments. With the wound data, Occupational Therapists successfully developed a cushion that can relieve the pain of pressure ulcers at a cost 20% of the market price.
Dr Sy also highlights the importance of patient empowerment in the initiative. “Sharing wound management knowledge with our patients and their carers has significantly reduced the frequency of wound redressing that many patients might otherwise need,” he says.
HKEC is currently the only cluster using this three-tier wound management system. In view of the expected rise in demand for certain services, the HKEC Quality and Safety Office and the Cluster Nursing Services Division set up the Working Group on Wound Management in 2008. The initiative enjoyed a positive response from a broad range of clinicians, including geriatrics specialists, surgeons, orthopaedic surgeons, nurse consultants, nurse specialists, frontline nurses, dietitians, occupational therapists and physiotherapists.
Year 2013
Health Care Food Service Team - PYNEH
Health Care Food Service Team - PYNEH

“Wow, this steamed fish is delicious.”
“The quality and temperature of the meals are good.”
“The hospital serves special fish soups to nursing moms helping them to breast-feed.”
Outsiders are always concerned about the catering services for patients. The Health Care Food Service Team of Pamela Youde Nethersole Eastern Hospital (PYNEH) began making revolutionary changes to its food-preparation methods and the quality of its catering services 17 years ago. The innovation started at PYNEH, which had just been opened at the time.
Clara Pi, the team’s leader says change began in 1996 when her team piloted cook chill technology in food production and later implemented cold-plating / end point retherm technology. This technology enables efficient production of safe quality foods in large quantities while maintaining nutrition. This new food production and meal service model became the new direction of the Hospital Authority’s patient food service.
They also worked with their IT colleagues to design, develop and implement the Dietetics Catering Management Computer System (DCMS). DCMS is a comprehensive system encompassing diet-order entry, food purchasing, production scheduling, menu planning and nutrient analysis. DCMS facilitated the standardisation of recipes and integration of regular and therapeutic diets. This system has now been rolled out to all hospital in HA.
Later, the team started to focus on the environmental impact of the nutrition of foods they serve to patients. They implemented a “meat replacement” programme in 2006, where textured soy protein replaced 30% of the meat in meat-cake recipes, and started the “meatless Monday” programme in 2010, in which money saved from buying meat is used to purchase organic vegetables for the patients. In 2011, they implemented the “meat reduction” Balanced Menu programme recommended by the WHO Healthcare Without Harm initiative. This enables the promotion of patient health and our environmental protection.
To reduce food waste, the team has worked with nursing and IT staff and has successfully cut down on meal tray waste from the wards and portions of rice. From 2011 to 2012, PYNEH saved a total of 42,157 kg of food, or an equivalent of HK$431,595.
Currently, the team provides 18,000 meals to 10 hospitals every day, making it the HA’s most effective catering department. Clara says special thanks are due to the great efforts of her colleagues in the kitchen, dietetics department, information technology services department, wards, receptor hospitals and the central food procurement department.
She also feels grateful to the first PYNEH Chief Executive, Dr Pamela Leung, and Mrs Mary Wan, Cluster General Manager (Administrative Services) at HKEC. “They supported me in implementing the new technology that has helped us to improve the quality of our meals, thus leading to today’s achievements.” The team will continue to pursue their mission on health and environmental protection in patient food service through innovation in a bid to assure patient satisfaction.
Year 2012
Hong Kong East Cluster Occupational Safety & Health (OSH) Team
Hong Kong East Cluster Occupational Safety & Health (OSH) Team

Making safety a priority, the Hong Kong East OSH Team set out to standardise an effective cluster-wide safety system. By appointing subject experts as work group leaders, the team identified some high risk hazards from chemical and radiation operation to workplace violence.
The team redesigned a comprehensive 3-tier OSH audit system, consisting of self inspection, third party cross-hospital audit and senior executive OSH walk-round, to enforce good practices. Communication is enhanced through a link person system of 150 people, regular staff forums and updated webpages.
Through self defense training and the use of restraining systems, workplace violence cases reduced by 38.2% in 2010 compared to 2007. Also, heat stress in Chai Wan Laundry was properly managed after the upgrade of the ventilation system. Thanks to the team’s effort, HKEC’s injury on duty (IOD) cases and IOD sick leave days reduced by 29.3% and 65.3% respectively in 2010 compared to 2005.
Team leader Mrs Mary Wan shared her tips on introducing new measures, “The key is to progress step by step, enhance communication by involving more frontline staff.” She wishes to thank each and every staff in the cluster for their teamwork and dedication in achieving towards “Helping People Stay Healthy”.
Year 2011
Enterprise Resource Planing Project Team - Hospital Authority Head Office and Clusters
Enterprise Resource Planing Project Team - Hospital Authority Head Office and Clusters
Enterprise Resource Planing Project Team - Hospital Authority Head Office and
Clusters
The task of the team was to replace HA's key finance, procurement and payroll systems. The scale, three-year duration, and the fact that all clusters would be affected, made it a complex, high-risk undertaking.
Despite many reported failures elsewhere, the team succeeded thanks to a massive joint effort of more than 50 contributing members and hundreds more, including front-line colleagues, and Oracle, the external partner.
The most outstanding achievement, however, was undoubtedly the teamwork, which required coordination, togetherness and sheer dedication to deliver.
The new systems provide a foundation for better working practices and increased future automation, with a far-reaching impact in terms of relationships. The cohesiveness, understanding and trust fostered between departments and across clusters has significantly improved communication to enhance daily operations and teamwork on future initiatives.
The task of the team was to replace HA's key finance, procurement and payroll systems. The scale, three-year duration, and the fact that all clusters would be affected, made it a complex, high-risk undertaking.
Despite many reported failures elsewhere, the team succeeded thanks to a massive joint effort of more than 50 contributing members and hundreds more, including front-line colleagues, and Oracle, the external partner.
The most outstanding achievement, however, was undoubtedly the teamwork, which required coordination, togetherness and sheer dedication to deliver.
The new systems provide a foundation for better working practices and increased future automation, with a far-reaching impact in terms of relationships. The cohesiveness, understanding and trust fostered between departments and across clusters has significantly improved communication to enhance daily operations and teamwork on future initiatives.
Year 2010
1. HA Rapid Diagnosic Laboratory Network on Influenza - Hospital Authority Head Office and Clusters
2. The Community Health Call Centre Team - HKEC
1. HA Rapid Diagnosic Laboratory Network on Influenza - Hospital Authority Head Office and Clusters
2. The Community Health Call Centre Team - HKEC
1.
HA Rapid Diagnostic Laboratory Network on Influenza shoulders an important responsibility in combating influenza pandemics by providing solid support to front-line clinical teams.
The Network was established in 2004 in preparation for outbreak of emerging infections, H5N1 avian influenza in particular. Its goal is to provide a specific etiological diagnosis for patient management and disease containment. Equipment, manpower and training, protocol development, reagents stockpile and quality of results have all been properly addressed.
The real challenge to the Network came in April 2009 when human swine influenza (HSI), with its unknown transmissibility and virulence, was spreading worldwide. The Network soon faced a sudden surge in requests for a specific diagnosis of HSI with a short turnaround time.
To meet this unprecedented service need, laboratories in the Network ran tests, virtually non-stop during the pandemic. They constantly shared experience, reagents and even equipment to ensure a high standard of performance. The number of laboratories under the Network grew from five to seven.
Members of the Network truly believe a rapid and accurate etiological diagnosis is the single most important element in shaping a positive outcome in patient management as well as the pandemic. With high morale and a high degree of professionalism, the Network will continue to contribute to the control of any upcoming pandemic.
2.

The Community Health Call Centre is a perfect example of a community-based service model to help high-risk elderly patients stay healthy after discharge from hospital.
Formerly the Telephone Nursing Consultation Service started in the Hong Kong East Cluster in 2003, the Community Health Call Centre Team has been providing an integrated comprehensive support service through a world-class hi-tech and hi-touch proactive tracking telephone support system. More than 15,000 discharged high-risk elderly patients have benefitted from the Team’s support since then.
The telephone support system is backed up by clinicians, nurses, information technology professionals, statisticians and ambulatory clinics in the HA, as well as non-governmental organisations and private doctors. This one-stop service bridges service gaps, monitors the situation of patients, provides timely interventions and referrals, and empowers patients and their caregivers to undertake self-management at home.
Three well designed evaluation studies have been conducted to find out whether the system met its objectives in detecting problems of patients at the earliest stage and reducing recurrent and unnecessary hospitalisation. A massive 25-50% drop in hospital utilisation and a decline in mortality have been consistently observed. In view of the encouraging results and positive feedback from patients, the system will be extended to eventually cover all seven clusters in the HA in the coming two years. There are also plans to expand the programme to benefit other patient groups.
Year 2009
Hong Kong East Cluster Quality & Risk Management Office
Hong Kong East Cluster Quality & Risk Management Office

The HKEC Quality & Risk Management (CQ&RM) Office was established in 2006 under the leadership of the Cluster Service Director, Senior Nursing Officer and Senior Hospital Administrator. Its role is to build an integrated management structure to formulate and drive quality and safety initiatives and to increase clinical and organisational effectiveness. To achieve this, it engages the key stakeholders at all levels who are responsible for quality standards and high-risk areas.
The Office has succeeded in creating clear reporting lines, a well-defined reporting format and a multi-communication flow between senior management, the Cluster Q&RM Committee, Functional and Divisional Committees. This enable information about quality and risk issues to flow between all the parties concerned in a more systematic way.
Participation and communication help to raise standards
The Office has already scored significant improvements in the following areas:
-
Strengthening the role of doctors by increasing their participationTo increase their involvement in incident and complaint management, a number of clinicians have been appointed as Department Q&RM Coordinators and Panel Specialists who participate in case reviews. This form of empowerment encourages clinicians to take ownership of quality and safety issues and to play a greater role in addressing them.
-
Enhancing learning and experience sharingA Cluster Incident Review Panel has been set up to strengthen the management’s focus on systems and processes in identified high-risk cases. A multi-channel communication system has also been put in place, so that lessons learnt can be shared with colleagues at various levels.
-
Training leaders for transformationDoctors now actively participate in designing, developing and implementing improvement programmes, such as correct patient identification, clinical handover and credentialing. The change process is creating leaders at all levels, thus helping to translate goals into operational realities.
Year 2006
Hong Kong East & West Cluster Family Medicine & Primary Health Care Services Team
Hong Kong East & West Cluster Family Medicine & Primary Health Care Services Team
Hong Kong East & West Cluster Family Medicine & Primary Health Care Services Team
The Family Medicine and Primary Health Care Services (FM&PHC) of Hong Kong East and West Cluster is a team of pioneers in rendering General Out-Patient Clinic (GOPC) service under the HA. The FM&PHC team has taken over 15 GOPCs on Hong Kong Island since July 2003 from the Department of Health and started devoting itself to Family Medicine and primary health care services.
Distributed all over the island as well as the remote islands, the GOPCs are governed by HKEC and HKWC. Whatever the colleagues are from ex-DH or the HA, they all work closely and cooperatively and strike for serving the public with quality primary care, especially for the socially disadvantaged, chronically ill population.
Since the take-over, the team has implemented diversified innovations to improve services such as introducing Clinical Management System (CMS) and Out-Patient Appointment System (OPAS) to GOPCs, launching patient hand-held record and executing new measures to eliminate patients queue. Appointments are then offered to chronic patients and pre-booking arrangement and phone-booking system instituted. The team also plays an important role in community health care by establishing communication channels between private primary care doctors and hospital specialists. The opening of Family Medicine Specialist Clinics (FMSC) helps better utilization of community resources through the triage function. With selfless dedication of the teammates, the primary health care services in the public sector is further improved and delivered straight to the public.
The Family Medicine and Primary Health Care Services (FM&PHC) of Hong Kong East and West Cluster is a team of pioneers in rendering General Out-Patient Clinic (GOPC) service under the HA. The FM&PHC team has taken over 15 GOPCs on Hong Kong Island since July 2003 from the Department of Health and started devoting itself to Family Medicine and primary health care services.
Distributed all over the island as well as the remote islands, the GOPCs are governed by HKEC and HKWC. Whatever the colleagues are from ex-DH or the HA, they all work closely and cooperatively and strike for serving the public with quality primary care, especially for the socially disadvantaged, chronically ill population.
Since the take-over, the team has implemented diversified innovations to improve services such as introducing Clinical Management System (CMS) and Out-Patient Appointment System (OPAS) to GOPCs, launching patient hand-held record and executing new measures to eliminate patients queue. Appointments are then offered to chronic patients and pre-booking arrangement and phone-booking system instituted. The team also plays an important role in community health care by establishing communication channels between private primary care doctors and hospital specialists. The opening of Family Medicine Specialist Clinics (FMSC) helps better utilization of community resources through the triage function. With selfless dedication of the teammates, the primary health care services in the public sector is further improved and delivered straight to the public.
Year 2005
Task Group on Public-Private Interface – HKEC
Task Group on Public-Private Interface – HKEC

The Team shares a common vision in achieving sustainable quality-driven health services in the Cluster – via the collaboration between the public and private health care providers. It has prioritized the medical services and identified public-private interface (PPI) opportunities systematically amongst a wide spectrum of public services. Ultimately it has turned members' insights and innovative ideas into practice for providing excellent medical service to the general public.
Since its formation in 2002, the team has launched various PPI programs such as triage and referral of new Specialist Out-patient Clinic (SOPC) cases to private sector, and Telephone Nursing Consultation Services for discharged elderly provided by Community Nursing Service (CNS). These projects have attained remarkable achievements.
Year 2004
Hong Kong East Cluster
Hong Kong East Cluster


Last year, PYNEH was among the first few hospitals with staff being infected with SARS. Yet, our SARS Team had demonstrated courage and strong commitment to provide quality care to the SARS patients.
All levels of staff worked cohesively to create a safe environment within a short period of time. This included the prompt conversion of some general wards into SARS wards with improved ventilation and active promotion of infection control measures and surveillance of practice. The spread of this unknown disease was thus rapidly under control in the Hospital.
At the clinical front, our Respiratory Physicians were able to develop an effective patient management protocol for SARS patients. The mortality rate of our SARS patients was among the lowest in Hong Kong and their recovery was also considered to be the most satisfactory. Through co-operation with other colleagues in Hong Kong, our SARS Team had contributed to publications on this disease in the medical literature.
Year 2003
Clinical Oncology Management Team – PYNEH
Clinical Oncology Management Team – PYNEH

The team has all along possessed high degree of cohesiveness and collaborated effectively to provide high tech and high touch service to patients. It is the first clinical department in PYNEH to obtain the accreditation of ISO 9001:2000 certificate and has strove for excellent benchmarking amongst the peers. To facilitate patients having a warm and relaxing atmosphere during receiving treatment, this team has enlisted support and donations from charitable and private organizations to arrange innovative improvements in environment and pioneered in introducing Visual Art concept to cancer therapy in Hong Kong.
Year 1997
1. Laundry Operation Transformation Team - Chai Wan Laundry
2. Comprehensive Paediatric Rehabilitation Centre - PYNEH
1. Laundry Operation Transformation Team - Chai Wan Laundry
2. Comprehensive Paediatric Rehabilitation Centre - PYNEH
1.

Through continuous communication, cooperation and teamwork, the Team has completely transformed the Laundry's work culture and practices, resulting in higher productivity and improved standards of cleanliness in its products. The Team also helped the Laundry gain ISO 9002 accreditation.
2.

The Centre successfully introduced an interdisciplinary one-stop integrated assessment service for handicapped children. In addition, it has worked in partnership with community organisations to bridge service gaps and integrate services. As a result, patients can now enjoy holistic care servicecs in a more convenient manner.
Year 1996
Admission Office - PYNEH
Admission Office - PYNEH

Customer service has been strenghtened by the team's initiatives in providing a one-stop enquiry service, introducing a mobile receptionist service, adopting an open counter design in registration counters, and designing slips to facilitate public inquiries. Despite the heavy demands of patients and visitors, its excellent reception counter and telephone services have consistently received appreciation from other hospital staff and the public.
HA Young Achievers
Year
Year 2025
1. Dr Man Man-yee, Associate Consultant (Intensive Care), PYNEH
2. Mr Rico Hung Hing-ming, Senior Radiation Therapist (Clinical Oncology), PYNEH
1. Dr Man Man-yee, Associate Consultant (Intensive Care), PYNEH
2. Mr Rico Hung Hing-ming, Senior Radiation Therapist (Clinical Oncology), PYNEH
1.
Dr Man has garnered multiple accolades in the field of medical research, with numerous publications in internationally renowned medical journals. She is equally committed to simulation-based education, spearheading the establishment of the Multidisciplinary Critical Care Simulation course to inspire and cultivate the next generation of healthcare professionals. Demonstrating innovation during the COVID-19 epidemic, Dr Man pioneered the use of prone positioning for critically ill COVID-19 patients, a groundbreaking approach that significantly lowered intubation risks and established an important model for clinical practice.
What extraordinary ability do you wish you had?
“Can we find out what he’s thinking or what he wants?” is a question I often hear from the anxious families of comatose patients. In those moments, I wish I had the extraordinary ability to read minds—to unravel the thoughts of patients and share their emotions with their loved ones, providing comfort and easing their concerns. Mind-reading would not simply guide treatment decisions; it would become a powerful bridge, connecting patients and their families during life’s most challenging times.
2.

Rico is a senior radiation therapist who leads the dosimetry team. He is actively engaged in the research in dosimetry and radiobiology. His studies on dosimetric comparison for the treatment of nasopharyngeal carcinoma and the radiobiological characteristics of FLASH-Radiotherapy have won awards at reputable international conferences, earning recognition from global experts in the field.
Please share a remarkable moment you experienced at work.
One evening in April 2024, when I had just finished my clinical duties and prepared to analyse my research data, I received an unexpected email — an invitation to join Sigma Xi, the Scientific Research Honour Society with over a century of history. Each year, this prestigious society confers membership only to a select group of individuals whose research has demonstrated significant impact. I am deeply honoured to become the first radiation therapist in Hong Kong to be invited to join Sigma Xi.
Year 2024
1. Dr Fergus Wong Kai-chuen, Associate Consultant (Department of Ear, Nose & Throat), PYNEH
2. Dr Jeffrey Yu Man-hin, Associate Consultant (Department of Surgery), PYNEH
1. Dr Fergus Wong Kai-chuen, Associate Consultant (Department of Ear, Nose & Throat), PYNEH
2. Dr Jeffrey Yu Man-hin, Associate Consultant (Department of Surgery), PYNEH
1.
Dr Wong was appointed as Rhinology Team head. His team cooperated with the university and developed the combined treatment of vitamin A and aromatherapy, to provide olfactory training for COVID-19 smell loss patients during the epidemic. Moreover, Dr Wong and his Head and Neck Surgery Team make use of clinical data and the innovative 3D printing technology in preoperative planning for head and neck cancer, which greatly increases the surgical outcome and success rate of surgery.
Share one of your memorable days at work and how did that day change your life?
That was the day when I performed a nearly total mandibulectomy and reconstruction surgery for a patient suffering from recurrent oral cancer. Since the patient had received radiotherapy and multiple flap surgeries previously, the surgical technique was very demanding, yet the only hope for the patient. After 23 hours, the operation was completed successfully. The success of an operation and a good recovery of patient are the greatest motivations for a surgeon. I will continue to enhance myself and provide high-quality treatment to my patients.
2.
The placement of ureteric stents is required for weeks after endourological surgery, which often causes irritation on patients. Dr Yu first introduced the adoption of magnetic ureteric stents which no longer relies on endoscopy or surgical procedures for the removal. This allows a speedy recovery for patients. He also introduced the transperineal Magnetic Resonance Imaging (MRI) fusion prostate biopsy technique to Hong Kong East Cluster, which increases diagnostic accuracy for prostate cancer with reduced complications.
What motivates you to work?
Seeing patients recover from illnesses is my greatest motivation. Meanwhile, being able to continue to develop, enhance and improve clinical services in areas that interest me, and to benefit more patients, encourages me to keep up the good work.
Year 2023
Ms Sy Yeung-wan, Associate Nurse Consultant (Urology), PYNEH
Ms Sy Yeung-wan, Associate Nurse Consultant (Urology), PYNEH

Ms Sy has been actively involving in the enhancement of urological care services, including the implementation of the trial wean-off catheter (TWOC) programme in the community setting to reduce inpatient and day-ward admission. She also cooperated with urologists to provide earlier preoperative screening for patients undergoing transurethral resection of prostate (TURP) to improve the cancellation rate of operation and shorten waiting times
What would you say to yourself 10 years from now?
I hope you could stay curious about urological care and keep growing and learning. Always bear in mind: “Develop a passion for learning. If you do, you will never cease to grow.” Keep concentrating on the development of urologic care and exploring new methods and techniques to improve the quality and efficiency of care. Be dedicated to your work, and do not forget your initiative of being a nurse in the first place.
Year 2022
Dr Jessica Law Yun-pui, Consultant (Obstetrics & Gynaecology), PYNEH
Dr Jessica Law Yun-pui, Consultant (Obstetrics & Gynaecology), PYNEH

If you were an object, what would you be?
A box of pastel colours. Pastel painting is my way to mediate and de-stress. The myriad colours reflect the multi-facets of my personality: the sense and sensibility. Through flexible mixing and matching of these colours or different sides of me, I can effectively deal with different challenges of everyday work and life.
Who inspires you in your work?
I am fortunate to have a father, who has taught me through his own example, how I could find both fulfillment and enjoyment in a busy work life. Being an obstetrician and gynecologist himself, he has inspired me to find meaning and satisfaction through earnestly helping and caring for my patients, and to always maintain a positive and calm frame of mind when faced with challenges. He has also helped me cultivate a range of interests to broaden my horizons and has reminded me to be curious, to enable me to better understand myself and others.
Year 2021
1. Dr Au Chi-lik, Resident (Ophthalmology), PYNEH/TWEH
2. Mr YEUNG Kai Jone, Advanced Practice Nurse (Intensive Care), PYNEH
1. Dr Au Chi-lik, Resident (Ophthalmology), PYNEH/TWEH
2. Mr YEUNG Kai Jone, Advanced Practice Nurse (Intensive Care), PYNEH
1.

What is your most memorable patient consultation?
I have once performed a cataract surgery on an old lady and when I conducted a post-operative follow-up with her, she suddenly took two bananas out of her basket and gave me as a token of gratitude. I was so surprised and felt so thankful. Besides, every word of thanks from a patient is the driving force of my work.
What is the most indispensable item in the workplace?
Slit lamp. It helps me focus on different parts of the eye and cure problems such as macula, optic nerve and retinal vessels. Also, it is a key tool to diagnose common causes of blindness among the elderly in Hong Kong.
What do you want to learn recently?
Artificial intelligence (AI). The COVID-19 pandemic has accelerated digitalisation in all walks of life, including the healthcare sector where development of smart hospital is the trend. We need to keep our fingers on the pulse of time, and learn AI, which will bring a revolutionary change to our society.
2.
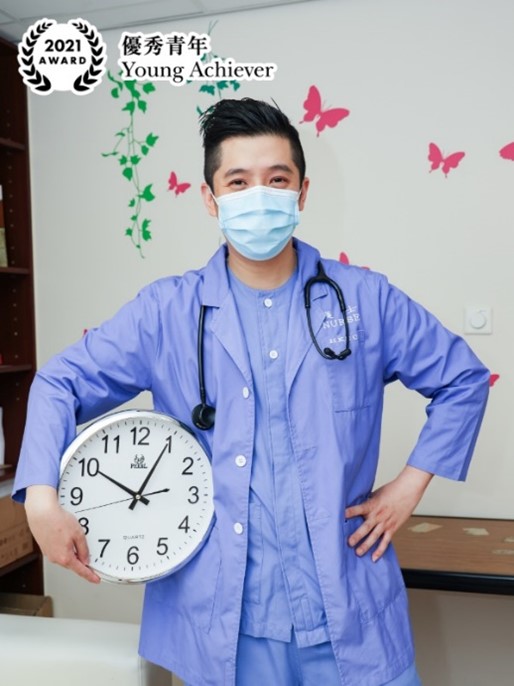
Share a habit at work.
I am tidy. I pack and organise all kinds of things including patient beds, equipment, and medical records, etc., before starting my work every day. I prioritise my work while tidying up so that I can complete all tasks as soon as possible and avoid being a ‘deadline fighter’.
How do you achieve work-life balance?
Work smart and make good use of your time. I used to spend most of my time studying and learning, but now I also need to take care of my family and accompany my children.
How do you overcome challenges?
When I get lost, I will share my worries with my wife or friends. The most important thing is to believe in myself and face the problems positively with my knowledge and past experience. I always remind myself that one’s attitude determines his altitude in life and life is full of ups and downs. Difficulties are just small setbacks in life.
Year 2019
Dr Daniel Wong, Consultant (Obstetrics & Gynaecology), PYNEH
Dr Daniel Wong, Consultant (Obstetrics & Gynaecology), PYNEH

Dr Daniel Wong’s aspiration of becoming a doctor originates from his father – Dr Wong Kin-ming, who was also a doctor in obstetrics and gynaecology. “It impresses me most that he still taught younger doctors at PYNEH in an honorary capacity even after he left the hospital and got sick later.” Influenced by his father, he determined to pass on his knowledge and skills to younger doctors.
Dr Wong and his team established Multidisciplinary Simulation and Skills Centre at Pamela Youde Nethersole Eastern Hospital from scratch in 2014, from programme planning, hardware arrangement, teaching, to even promotion. “Patients today are reluctant to consult green doctors. But how can these doctors gain clinical experience if they don’t have the chance to attend to patients? Simulation training is indeed necessary to build up doctors’ confidence and enhance patient safety.”
To become a consultant at the young age of 35, one needs more than luck. It is the faith that brings Dr Wong to this position. “I see every task a valuable learning opportunity,” he says. For instance, he was asked to restructure the urogynaecology service, which is not a popular subspecialty. It serves female patients aged 60 to 90 who suffer from uterine prolapse and urinary incontinence. Few doctors are interested in this area because of the complex surgery. Yet Dr Wong does his best for the well-being of elder patients. “When patients tell me that their quality of life has improved and can even travel on their own, it is encouraging and it reminds me of my resolution to become a doctor.”
Year 2018
1. Mr CHIN Yi Ma, David, Occupational Therapist I, Occupational Health Centre (HKEC)
2. Dr Thomas Fung Tai-hang, Consultant (Ear, Nose & Throat), PYNEH
1. Mr CHIN Yi Ma, David, Occupational Therapist I, Occupational Health Centre (HKEC)
2. Dr Thomas Fung Tai-hang, Consultant (Ear, Nose & Throat), PYNEH
1.

Occupational Therapist I David Chin is a ‘master key’ in the eyes of his colleagues. Not only does he excel in his own expertise, but he is also active in promoting occupational safety. He is a core member of the cluster’s Occupational Safety and Health (OSH) working groups, such as slip, trip, fall and struck working group, where he strives to create a safe and healthy working environment for fellow co-workers.
To strengthen OSH knowledge, David obtained a Master’s degree in Occupational Hygiene and subsequently enrolled himself in a specialised training course on staircase safety assessment in the Britain in 2016. “The height, depth and slip resistance of each step and the lighting of the surrounding environment of a staircase can affect user safety.” After his return to Hong Kong, he has performed onsite comprehensive assessments on 41 major staircases in all hospitals of the Hong Kong East Cluster (HKEC), such as the stairs near the mini-bus stop at Pamela Youde Nethersole Hospital and the entrance of Wan Chai Road at Ruttonjee Hospital. He has made 111 suggestions following the inspection and communicated with the management team of each hospital and cluster’s Facilities Management Team to ensure that fellow co-workers can benefit from the improvement plans and work in a safe environment.
He always reminds colleagues of the concept of OSH, “For example, frontline colleagues are suggested to stretch for five to 10 minutes before they start working to avoid neck and back pain; those working in laboratories are encouraged to use gadgets to open capsules to reduce the risk of repetitive wrist injury.”
Apart from the OSH duty, David also deals with cases of injury-on-duty involving colleagues from the HKEC and civil servants at the HKEC Occupational Health Centre. He says, “An occupational therapist doesn’t only help patients recover physically, but also help them restore self-confidence to return to work.”
He recalls the case of a former patient, “I remember a patient from the Special Duties Unit of Hong Kong Police who was injured during tactic training in which he had to carry heavy equipment and a colleague who weighed similar to him to run upstairs. I designed simulation training for him to carry a number of heavy items and walk up and downstairs and the weight is gradually increased to the level that matched with his work requirements to help him rebuild his self-confidence and return to work.”
2.

The outbreak of SARS in 2003 made the then intern at ward 8A Dr Thomas Fung a patient, a switch in role that allowed him to understand the needs of patients even better and constituted his present self – a doctor who spares no effort in saving lives.
“I’ll always remember the heartfelt warmth from the simple greeting my attending doctor and mentor, Prof Joseph Sung Jao-yiu, gave me every day when I was in severe conditions. It also reminds me of a principle I shall uphold – heal from the heart. My vision of being a doctor is that I don’t care about the number of surgeries have done or money. The most important is giving a patient the only chance to live,” he says.
How committed is Dr Fung to saving lives? He once rushed back to the hospital when he was on call to operate on a patient of tonsil cancer who had sudden bleeding and was under the danger of suffocation in the midnight, after which he stayed behind till the conditions of the patient stabilised. He also worked as a part-time doctor at the Accident & Emergency Department of Pamela Youde Nethersole Eastern Hospital and Prince of Wales Hospital to absorb experiences while enjoying the quest for knowledge beyond his own speciality. Moreover, he takes a five-day leave every year in summer since 2012 to teach at his mother school, “I analyse and share real cases with my juniors, which I believe would also be a great way to learn and consolidate my own expertise.”
Dr Fung has completed several hundred major head and neck surgeries, including head and neck tumour excision, and free flap transfer, most of which he could finish in half of the expected time, which is how he earned himself the name of ‘the most efficient surgeon’ from his colleagues. However, he still felt immensely stressed when he was to carry out surgery of paranasal sinus on his close friend at university who is now a pathology doctor. “I was afraid of losing a good friend in case of any slips. The surgery was concluded smoothly and my friend is currently under recovery; I’m just really glad that I can save the life of someone I’m close to.”
He emphasises, “We should take up our courage and go all in to save lives when we’re able to.”